IRIS Background Check Information
PremierFMS is required to complete an IBC, or IRIS Background Check, for all applicants and existing Participant-employed providers every 4 years, or as needed. The below explains how the results are reviewed and determined.
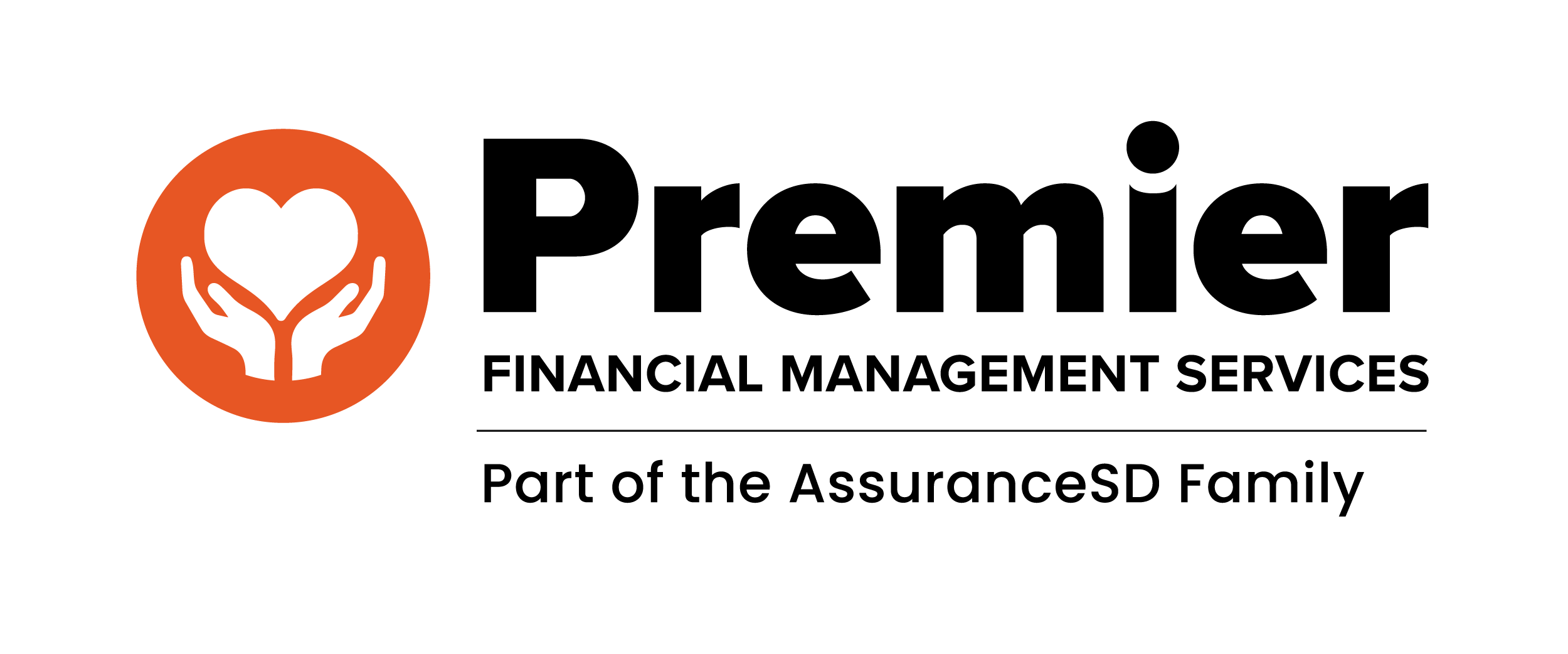
Table 1: Caregiver Misconduct Findings will disqualify an applicant or existing Participant-employer provider from receiving Medicaid reimbursement for IRIS services. Caregiver Misconduct Findings are not appealable. The Participant and applicant or Participant-employer provider may request a Rehabilitation Review from DHS.
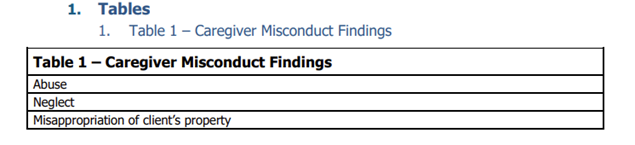
Table 2: Serious Crime convictions will disqualify an applicant or existing Participant-employer provider from receiving Medicaid reimbursement for IRIS services. Serious Crimes are appealable. The Participant may submit an appeal on behalf of the applicant or Participant-employer provider from DHS
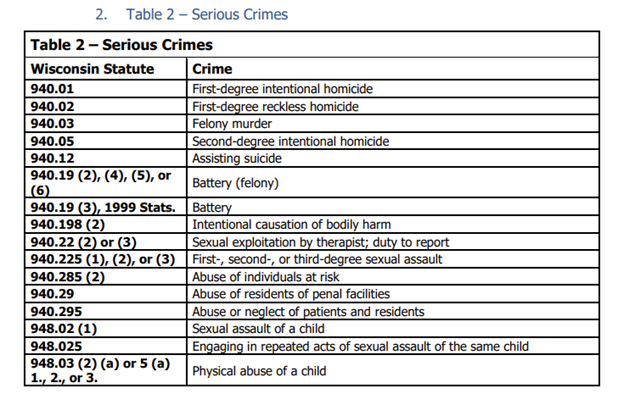
Table 3: Mandatory Disclosure Crimes will not determine the qualification status of the applicant or Participant-employed provider to receive Medicaid reimbursement for IRIS services. However, PremierFMS is required to report them to the Participant so the Participant can make an informed decision about who provides their care.